I am no stranger to pain. We have developed an intimate relationship over the years. From fingers closed in moving cab doors to natural childbirth, bone breaks requiring more hardware to be installed than my kitchen cabinets and ruptured, gangrenous appendix removals I could always be assured of one thing – whatever the pain was at the time, it would end. Enter a different pain. An unrelenting pain that accompanied me through my waking moments and invaded my dreams at night. A pain that became something I could rely on through the years that slowly over time took away more and more of the things that bring me enjoyment.



Say hello to osteoarthritis of the hip. I have had hip pain since my late 30s. Numerous years ago I described to my then primary care doctor what I was experiencing and he took an x-ray, told me I had some ‘mild’ arthritic changes in my hip, poked and prodded me then figured out I had some serious bursitis. Home I went on non-steroidal anti-inflammatory medication (Motrin). It helped and I stopped taking them. It’s important to note that I didn’t say, “It went away”. I said, “It helped”.
A medical literature search (yes, I can still do that) revealed that chronic pain, “negatively impacts multiple aspects of patient health, including sleep, cognitive processes and brain function, mood/mental health, cardiovascular health, sexual function, and overall quality of life. Furthermore, chronic pain has the capacity to become increasingly complex in its pathophysiology, and thus potentially more difficult to treat over time.” (If you want the reference citation I’ll be happy to provide you with it.) As time went on I began to have more consistent episodes with hip pain. A planned trip to China for 2 weeks which would entail a lot of walking precipitated me to visit my doctor and get a cortisone shot. This also worked well and got me through China. Soon I became more dependent on Naproxen and would take it regularly until my stomach started to bother me and then I would quit for a couple of weeks until the pain outvoted the health of my gastric mucosa. Years passed and I went from being able to easily knock out over 5 miles a day to barely being able to do 2 without a significant limp. By this time I had a new primary care doctor who did another x-ray and said, “Why don’t you try physical therapy?” He recommended some local PTs and I settled on a solo practitioner instead of a large group. I had a consult that lasted about 2 hours which included a thorough history and physical assessment at the end of which I was told, “I can’t help you. You need a hip replacement.”

Off I go for a consult with a very well known and highly recommended joint replacement “clinic” in Northern Virginia. They do (another) x-ray, the resident does a brief history and less than 5 minute physical. The attending physician comes in and tells me I have osteoarthritis of my hip and presents me with treatment options which include a more involved pain injection (no thanks) but he feels I am not taking a high enough dose of non-steroidal anti-inflammatory medication and suggests a new dosage. They say a hip replacement is in my future but probably at around age 70 (average age they tell me is 72). “How will I know when?” I ask. “You’ll know” he responds and off I go with a new Rx.
Fast forward another 2 years. Covid hits and a major part of our activity becomes walking on our mountain, gardening, landscaping and hitting our pool in the summer. All of these things become more painful and I am hobbled to some degree depending on the day. After a while, it no longer depends on the day. The Naproxen is once again bugging my gut, my flexibility is almost non-existent and my lower back plagues me with sciatica. I transition from a very physically active job to a sedentary one. I return to my primary care doctor for an overdue annual exam and he inquires about my hip. I tell him that I am frustrated beyond belief as I enjoy activities that I find increasingly hard to perform. I tell him I’m going to search for a female orthopedic doctor because maybe my issues are related to the supporting structures of my back and pelvis. He offers a suggestion to see a surgeon who specializes in hip & knee replacements. My doctor knows a fair number of doctors who have seen this guy all with good results. Sure, I’m game.

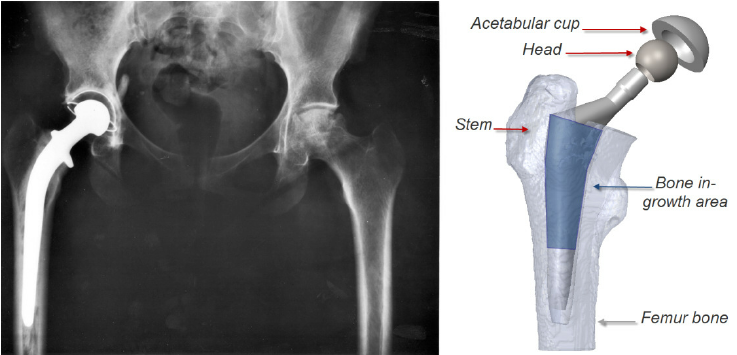
I arrive at the office and the first thing they do is take an x-ray. (Marie Curie was exposed to less radiation than I.) The surgeon enters and I tell him my tale. He shows me my x-ray (I am now pretty good at reading them) and tells me that all of my woes are related to my obvious hip arthritis which is now practically bone on bone in one area. He states that since I have been dealing with this for quite some time and have employed several of the key mitigation strategies used to treat the disorder we could continue with those treatments. He advises me that this will continue to worsen. We have a discussion about quality of life and my concerns that maybe I’m ‘too young” for hip replacement surgery. He tells me he recently performed a total hip replacement on a 35 yr old and average life of the replacement parts is about 30 years. I inquire about more specifics of the procedure itself. He says it would be done as a same day surgery, I would be up and walking after about an hour and would do my physical therapy at home. Further discussion ensues as I delve more specifically into materials, technique, risk, benefits, . . I won’t bore you with those details. At the end when I am satisfied he tells me that this is elective surgery and if I decide this is the route I want to take to let him know. I express that I wish to mull it over and discuss with my husband.

I decide to have a total hip replacement. My doctor’s office is a well oiled machine. I speak with his assistant who forwards my information to their scheduling person who puts me in touch with their finance department who calls my insurance company to verify my coverage. I receive an email from the total joint replacement specialist at the hospital I plan to have my surgery in and she gives me a power point presentation since mandatory classes have been suspended due to Covid. I have a virtual pre-op with the PA who will be assisting on my surgery and get all my medications prescribed and preauthorized.
Don picks up a cane, walker and elevated toilet seat from our local hospice. We know they lend this type of equipment because when Darren had his knee done our local hospital informed us of this valuable service. I have to have a Covid-19 test before surgery. I inquire if I can decline this since I am fully vaccinated and am informed that I can decline but they will decline to perform my surgery. I suggest they have their infectious disease department review the most recent studies. I wind up having 3 Covid tests: 1 for my pre op, 1 because I get sick right before my surgery and want to make sure I don’t have Covid and another before my rescheduled surgery.
I am given instructions to shower for 3 consecutive days before my surgery with a special cleanser and wear clean pajamas and have clean bed linens. I am given 3 Gatorade type beverages which I must consume the evening before and the morning of my surgery to keep me hydrated and provide some calories. I arrive the morning of my operation and get prepped for surgery. The Same Day Surgery staff at HCA Stone Springs Hospital are wonderful and I feel as comfortable as I can considering I am about to have my leg cut off and reattached in a short period of time. (This is how my son, Matthew, continuously refers to my surgery which results in my mind actually picturing this.)
I speak with the anesthesiologist and inform him that I am fine with a spinal but don’t want to hear any tools being used (to cut off my leg). He assures me that I won’t. Don decides he doesn’t want to have to sit around with a mask on and decides he will wait in the car until I am in recovery but then can’t go through with that plan and stays by my side until they wheel me into the OR.

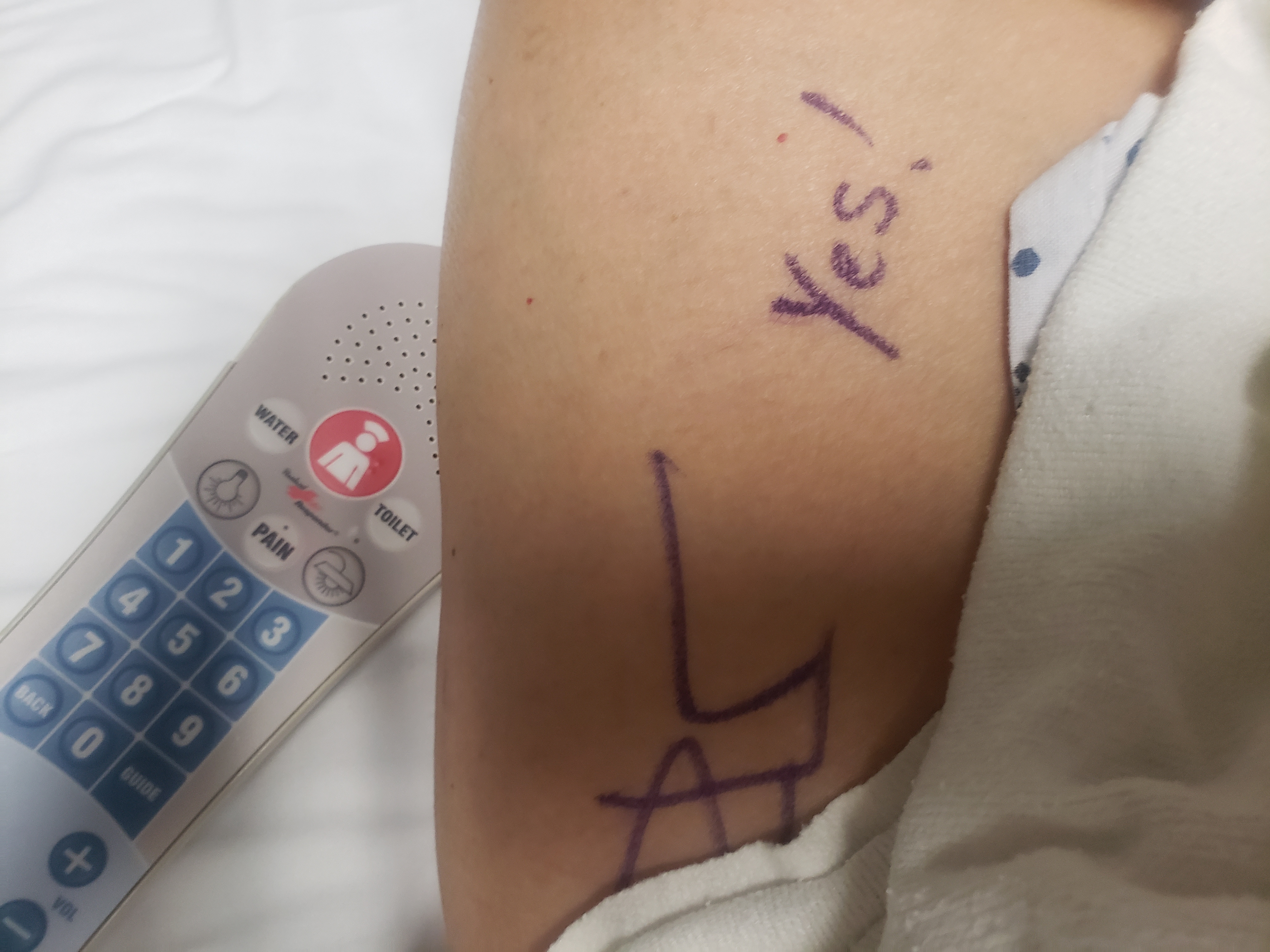
I am wheeled into the OR at noon. I do recall sitting up for my spinal and having a conversation with the person who is supporting me about my tattoo. I have recollections about describing how I got it in Bangkok and then I remember no more until I heard, “Mrs. Russo, wake up.”
As I am being wheeled into the recovery area I see a clock on the wall and it says, 1:20 pm. How the hell do they do all that in about an hour? I had an anterior approach hip arthroplasty (technical name). In this procedure there is less muscle trauma as the muscles aren’t cut but instead are separated along the natural plane (with retractors by guys the size of lumberjacks), this results in less pain, quicker mobility, less risk of hip dislocation, less limping and shorter hospital stays.
- The surgeon makes a cut in front of your hip joint.
- The surgeon separates your muscles to see your hip joint.
- The surgeon removes the upper part of your femur (thigh bone) and the damaged cartilage and bone from your pelvis.
- The surgeon replaces your acetabulum (hip socket) and the head, neck, and part of the shaft of your femur (thigh bone) with an artificial joint. In my case the hip bone socket was lined with a plastic type cap, the ball joint was ceramic and the shaft that goes into the thigh bone is titanium.
- The surgeon uses X-ray & fluoroscopy to make sure the joint is in the right place.
- The surgeon or an assistant will close up the incision. My sutures were all internal and I had a waterproof occlusive dressing on for 2 weeks.
After the first hour while they insured I wasn’t going to die I was visited by the physical therapist who got me out of bed and walking with a walker. She walked me down the hall to a free-standing flight of stairs and taught me how to go up and down with the walker and explained the difference of doing it with a cane. When she was finished, the occupational therapist came in and demonstrated some assistive devices I was being sent home with to make it easier for me to function: Grabbers for picking up things like clothes & shoes and a different type for getting things out of cupboards, a very cool yet very simple device to help me put my socks on and a very sturdy, long shoe horn. My last visit was with the total joint replacement specialist RN who went over all the exercises I’d be doing at home for my physical therapy. The spinal has now worn off and I can pee. I am in my car and headed home at 4:00 pm.


I am on a drug regimen of 7 different medications. When I am finished with the antibiotics I start probiotics to help my gut recover. I stop the narcotic after 4 days because it is wreaking havoc with my gastrointestinal tract & lots of ice and the other drugs are seeming to manage my pain well. Interesting point: my insurance company would not approve 60 oxycodone and would only give me 45 tablets of which I used about 11. Gotta love the opioid epidemic! I get up about every hour during the day and walk 10 laps in my hallway & do my exercises twice daily. I seem to be sleeping OK despite having to sleep on my back. Before surgery I invested in one of those U-shaped body pillows and my sister sent me a knee pillow and these keep me pretty comfortable. The first 2 days I use a walker then switch to a cane. After the first week I am only using the cane outdoors or at night to get up to pee.


When I return for my 2 week post op check up I am averaging about 3000 steps/day. If I go too much over that my lower leg swells up. I am able to put my own socks on & tie my own shoes. (It’s a big deal after total hip! Shout out to all the 6 yr olds, it’s not as easy as you’d think!) My Physicians Assistant says I’m what they call “A good patient”. My ‘hippie support group’ declares me a rock star. I know that being in pretty good health & shape pre op gave me a ‘leg up’ (pun intended).


Don was ever by my side for 3 weeks. I know he was not thrilled when I got rid of the cane after a few days at home, started gardening (no bending or squatting), went down 13 stairs at home (oh wait, he didn’t know about that), insisted I could put on my own socks and shoes and wanted to go on ever increasing walks. True to form he has always supported me in all my decisions, even if he doesn’t necessarily agree with them. My other constant companion who insisted on lying on me continuously for the first 2 weeks post op and provided me with much comfort was one of my cats. (Not you, Wicked, you hateful bitch.) My boy Ozzy never left my side. In fact, he insisted on lying on my affected leg.

I am now 3 1/2 weeks post op. I can walk a little over 3 miles/day and my pace is improving at a steady rate. My biggest problems now are remembering that I can’t do certain things yet like cross my legs, kick my operated leg backwards or bend over/squat for prolonged periods. The constant pain I had in my hip is gone (my only discomfort is surgery related now) and my sciatica and lower back pain has disappeared. (I can only assume it was related to compensating for my bad hip.) I don’t know if my results are typical. I can only tell you my truth. My next check up is at 6 weeks post op and I’ll have (you guessed it!) another x-ray to see that everything is where & how it should be and at that point I should be cleared for the hot tub & pool! Down the road I’m thinking about learning to ride a bicycle again. (Do you ever forget? It’s been like 40 years.) I also have a date for a hike with my son, Eric. I told him to pick one with a great overview at the finish that makes me look like a badass but that’s not too hard. Happy trails to you!


 Follow
Follow
2 Responses to Susan Gets A New Hip